Geoffrey Mosoti Nyakiongora
Geoffrey Mosoti Nyakiongora is a Graduate Architect from Nairobi, Kenya and a Master of Science in Architecture + Urbanism candidate at the Massachusetts Institute of Technology (M.I.T.) . He holds undergraduate degrees in Architecture, Architectural Studies and a graduate degree in Advanced Architectural Design from the University of California - Berkeley.
His interests lay in a vast number of topics including sustainable design, simulation, architectural history, urban forms and blockchain. His work on urban forms and sustainability in Kenya led to his invitation to work with Rem Koolhaas, OMA and AMO on "Countryside: The Future" project from 2017-2020. The research focused on the field of countryside and rural forms and their gradual and progressive evolution over the years, Geoffrey was selected as one of the lead researchers and coordinators for the Kenyan team and ultimately presented their work at the Solomon R. Guggenheim in New York in the year 2020.
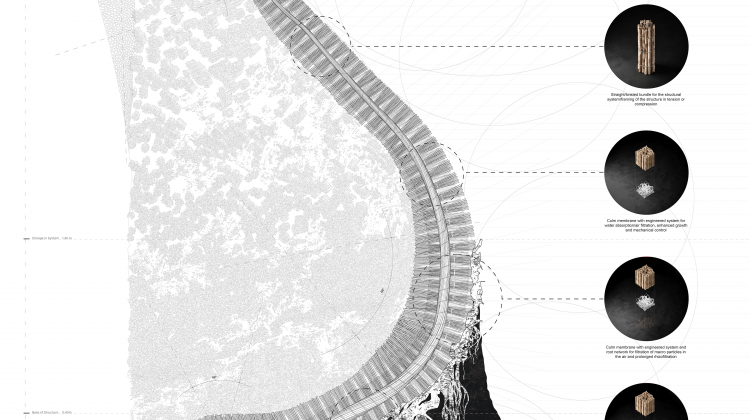
His research at U.C. Berkeley focused on the use of biomimicry, biomimetic systems and materials to solve issues in indoor air quality and potentially enrich natural eco-systems. Together with his team, his research won two prestigious awards, the AIA Award 2022 for Best Student Design Project and the Detail Design Award 2022 for best student project. He is also a 2024 Morningside Academy of Design Fellow. The Morningside Academy of Design is the most prestigious design fellowship throughout the Massachusetts Institute of Technology.
Geoffrey has also worked as a graduate architect and designer in a set of diverse projects in private practice in Kenya and has taught at the Department of Architecture and Building Science at the University of Nairobi and as Graduate Student Instructor at U.C. Berkeley.

The proposal is envisioned to be designed and built for and by the local community of Kabete.
The project will cater to over 5,000 customers daily and provide employment for over 500 vendors. The design also seeks to integrate the community in its construction to create means of employment for the local community.

is essential in safeguarding the well-being of a country’s citizens. Kenya's doctor-to-patient ratio is a staggering 1:5,725, far exceeding the recommended 1:1,000 ratio, according to the WHO. This means that the vast majority of Kenyans do not have access to any form of medical care and many who do have to struggle to access it. Another glaring issue plaguing Kenya's healthcare system is the lopsided allocation of medical personnel, facilities, and equipment - with urban centers enjoying a high amount compared to rural areas. Though the geographic dispersion of nurses is more equitable than doctors, their overall numbers across the country still fall short of the 25 per 10,000 population ratio recommended by the
World Health Organization for adequate healthcare provision. This skewed urban-rural divide leaves many Kenyans residing in remote or impoverished rural regions grappling with little to no access to essential medical services and expertise available to their urban counterparts, highlighting an acute need to address this inequitable distribution of vital healthcare resources. A recent health facilities census by the Ministry of Health revealed that 93% of over 12,000 facilities are unable to provide basic outpatient services due to lack of equipment. 78% of these facilities cannot offer critical care, with a paltry 2,304 public ICU/HDU beds serving a population of 50 million people! For maternity services, 84% of around 5,000 facilities lack essential equipment. This has led to a shocking number of Kenyans dying due to poor facilities and medical negligence. With over half of health facilities being in urban areas where only 30% of the population resides, cases of alleged medical negligence resulting in deaths have occurred even in major urban hospitals. This shortage of new professionals further strains Kenya's ability to meet its healthcare demands. Rural public health facilities, where most of the population resides, routinely grapple with funding
shortfalls and resource scarcity. Simultaneously, the draw of higher compensation packages and superior infrastructure lures healthcare workers away from rural postings towards more lucrative urban opportunities. This rural to urban migration deepens the disadvantages already faced by underserved regional populations in accessing quality care. This research seeks to assess if AI could also aid in designing the functional requirements and layouts of these new rural hospitals based on local health needs, climate, and culture. The study also seeks to investigate if harnessing AI across planning, design, construction and resource management, stakeholders in Kenya’s healthcare sector could leapfrog conventional methods to build a new network of high-quality rural hospitals rapidly and cost-effectively. This could drastically increase healthcare access for underserved populations and help alleviate the urban-rural facility divide.



